Everything starts with the pevic nerves. We “lost” them in 1945 when we started using formalin to preserve them (instead of alcohol). There are two handfuls of nerves on either side of your pelvis – they are vulnerable to injury in labour, straining on the toilet or through surgical procedures.

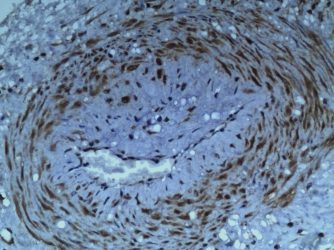
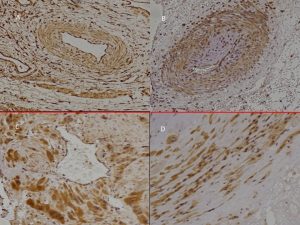
(1) The lower half of the pregnant uterus contains injured nerves in a “halo” around thickened arterioles (blue vessel). The nerves do not extend to the placental bed but a “halo” of hyalinised cells (white) does so (pink vessel).
(2) Injured nerves induce purinergic, P2X3, “stretch” receptors (brown) in arteriolar walls (“early-onset” PET) and myometrium (“late-onset” PET).
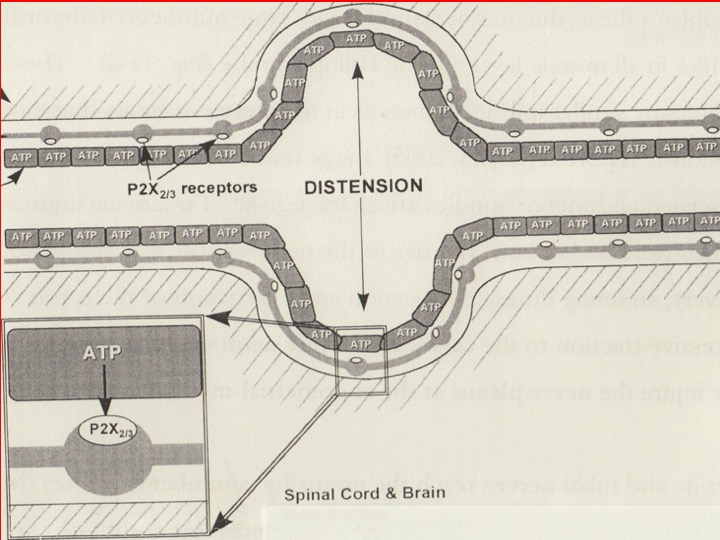
(3) Stretching injured uterine tissues releases proteins e.g. s-flt1, PlGF, etc and ATP. ATP is the neurotransmitter at purinergic “stretch” receptors that initiates a reflex between the uterus and kidneys (uterorenal reflex) that redistributes renal blood flow.
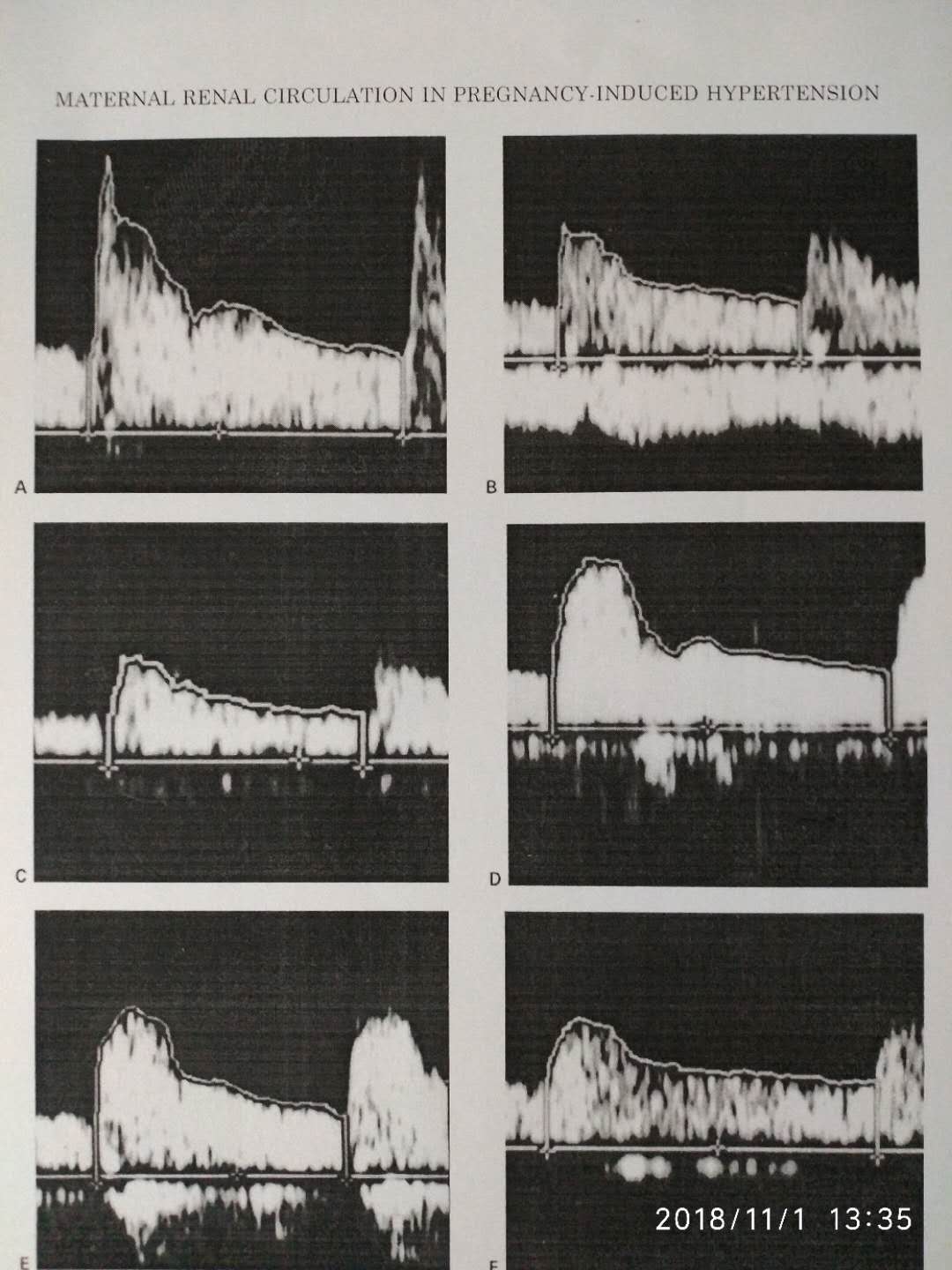
(4) Maternal renal artery waveforms show normal flow through different smaller arteries (A-C) but in preeclampsia (D-F) that flow is diminished. Pre- and postpartum waveforms provide evidence for a renal corticomedullary shunt in preeclampsia.
Proving all three elements of the pathway – P2X3 receptors, uterorenal reflex and renal corticomedullary shunt – may best be achieved by carrying out maternal renal artery Doppler studies during a Caesarean section. One might expect to see restoration of normal, maternal renal artery waveforms shortly after delivery of the baby (removal of the “stretch” stimulus”). Biopsy of the uterine lower segment (no need for placental bed biopsy) may demonstrate the concurrent presence of “purinergic”, P2X3 receptors (or, it may not).